Tuberculosis Hotspots in Nepal Linked to Environmental Factors
Table of Contents
- 1. Tuberculosis Hotspots in Nepal Linked to Environmental Factors
- 2. TB Prevalence Clusters: A Geostatistical Analysis
- 3. Key Takeaways:
- 4. Environmental Factors: Temperature, Land Use, and Rainfall
- 5. Land surface Temperature
- 6. Land Use Patterns
- 7. Rainfall patterns
- 8. Implications and Actionable Advice
- 9. Analyzing the Correlation Between Environmental Factors and Tuberculosis Prevalence in Nepal
- 10. Land Surface Temperature and Tuberculosis Prevalence
- 11. Land Surface Temperature Day
- 12. Land Surface Temperature Night
- 13. Cropland Distribution and Tuberculosis Prevalence
- 14. Urbanization and Tuberculosis Prevalence
- 15. Mapping Tuberculosis: Urbanization, Precipitation, and Spatial Analysis in Nepal
- 16. Urbanization and TB Prevalence: A Growing Concern
- 17. The Role of Precipitation: Unpacking Environmental Influences
- 18. Statistical Modeling: Quantifying Influences
- 19. Implications and Actionable Insights
- 20. Given the article’s focus on environmental factors contributing to TB prevalence in Nepal, what specific policy recommendations could be implemented to mitigate the impact of climate change on TB transmission?
- 21. Tackling Tuberculosis in Nepal: An interview with Dr. Anya Sharma
- 22. Understanding TB hotspots in Nepal
- 23. The Role of Environmental Factors: Temperature, Land Use, and Rainfall
- 24. Targeted Interventions and community-Based Programs
- 25. The Impact of Urbanization on Tuberculosis Transmission
- 26. Research and Future Directions in Tuberculosis Control
- 27. A Final Thought: Encouraging Community Involvement
Tuberculosis (TB) remains a significant public health challenge in Nepal, with prevalence rates varying significantly across different districts. Recent data from fiscal years (FY) 2020-2023 reveals distinct patterns in TB prevalence, coupled with notable environmental factors that may contribute to thes trends.Understanding these correlations is crucial for targeted interventions and effective public health strategies.
TB Prevalence Clusters: A Geostatistical Analysis
Geostatistical analysis using Gi* statistics highlights areas with significantly high and low TB prevalence. In FY 2020–2021, districts such as Banke, Rupandehi, Parasi, Parsa, Bara, Rautahat, Mahottari, Makawanpur, Lalitpur, and Kabhrepalanchok exhibited high TB prevalence. Conversely, Mustang, Kaski, Solukhumbu, Okhaldhunga, Bhojpur, Sankhuwasabha, Terhathum, Taplejung, and Panchthar showed low prevalence.
This pattern shifted slightly by FY 2021–2022. While Banke, Kapilbastu, Parsa, Bara, Rautahat, Mahottari, makawanpur, Lalitpur, and Kabhrepalanchok continued to report high TB prevalence, the districts with low prevalence remained largely consistent: Solukhumbu, Okhaldhunga, Bhojpur, Sankhuwasabha, Terhathum, Taplejung, Panchthar, and Dhankuta.
The latest data from FY 2022–2023 indicates a further expansion of high prevalence areas to include Banke, Kapilbastu, Parasi, Parsa, bara, Rautahat, Sarlahi, Mahottari, Makawanpur, Lalitpur, Kabhrepalanchok, Bhaktapur, and Nuwakot. Low prevalence continued in Mustang, Kaski, Solukhumbu, Okhaldhunga, Bhojpur, Sankhuwasabha, Terhathum, Taplejung, Panchthar, and Jhapa.
Key Takeaways:
- Consistent Hotspots: Banke, Parsa, Bara, rautahat, Mahottari, Makawanpur, Lalitpur, and Kabhrepalanchok consistently report high TB prevalence across all three fiscal years.
- Stable Low-Prevalence Areas: Districts such as Solukhumbu, Okhaldhunga, Bhojpur, Sankhuwasabha, Terhathum, and Taplejung consistently exhibit low TB rates.
- Emerging Areas of Concern: Sarlahi, Bhaktapur, and Nuwakot show an increase in TB prevalence by FY 2022-2023, warranting further investigation.
Environmental Factors: Temperature, Land Use, and Rainfall
Environmental factors play a crucial role in influencing disease prevalence. Analysis of Land Surface Temperature (LST), land use patterns, and rainfall reveals potential correlations with TB incidence in Nepal.
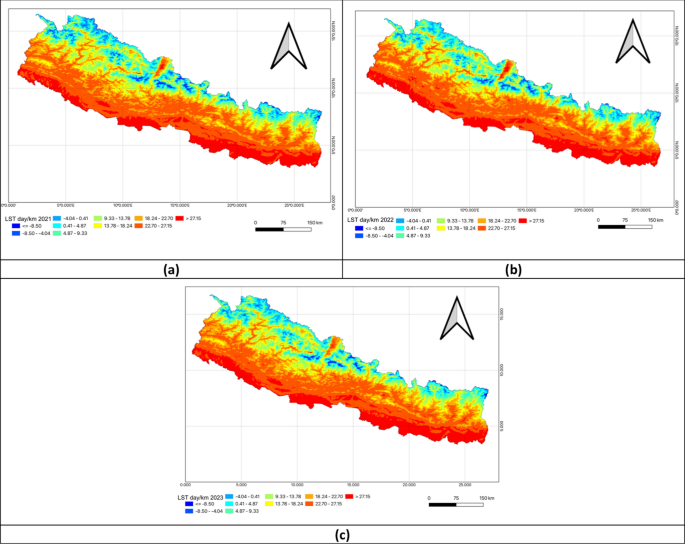
Land surface Temperature
Nepal’s diverse topography results in significant temperature variations. The southern lowland Terai region experiences warmer daytime temperatures due to its lower altitude, while the northern Himalayan regions remain cooler due to higher elevation and snow cover. These temperature gradients can impact the survival and transmission dynamics of Mycobacterium tuberculosis, the bacteria responsible for TB.
Analyzing Land Surface Temperature during the day “highlighted the stark temperature differences influenced by elevation: the southern lowland Terai region experienced warmer daytime temperatures due to its lower altitude while the northern Himalayan regions remained cooler becuase of higher elevation and snow cover.”
Nighttime Land Surface Temperature (LSTN) also follows a similar pattern, with the southern plains consistently experiencing warmer temperatures and the northern mountainous regions remaining cooler. These consistent temperature patterns may influence human behavior, such as indoor crowding during colder months, perhaps increasing TB transmission.
Land Use Patterns
Land use patterns,specifically the proportion of cropland and urban areas,also correlate with TB prevalence. the southern Terai region has a higher percentage of cropland, while the northern mountainous regions have minimal cropland.
Urban areas are predominantly located in the southern and central parts of the country. Higher population density in these urban centers, coupled with potential factors like air pollution and socioeconomic disparities, may contribute to increased TB transmission rates.As illustrated, the percent of total cropland area and the percent of total urban areas are key factors. As stated, “urban areas were predominantly located in the southern and central parts of the country while the northern mountainous regions showed minimal urban advancement.”
Rainfall patterns
Rainfall patterns exhibit significant regional variations. Northern Nepal experiences lower rainfall, while the central and southern regions receive higher precipitation levels. Increased rainfall can lead to flooding and displacement, potentially disrupting healthcare services and increasing the risk of infectious disease outbreaks, including TB.
The data shows that “While northern Nepal consistently experienced lower rainfall, central and southern regions saw higher precipitation levels, especially in FY 2022–2023 where rainfall intensified.”
Implications and Actionable Advice
Understanding the spatial distribution of TB prevalence and its association with environmental factors is crucial for developing targeted interventions. Public health officials and policymakers should consider the following:
- Resource Allocation: Prioritize resource allocation to high-prevalence districts such as Banke,Parsa,Bara,Rautahat,Mahottari,Makawanpur,Lalitpur,and Kabhrepalanchok.
- Environmental monitoring: Implement continuous monitoring of environmental factors, including temperature, rainfall, and air quality, to predict and mitigate potential TB outbreaks.
- community-Based Programs: Strengthen community-based TB screening and treatment programs, especially in densely populated urban areas and regions with high cropland density.
- Climate-Resilient Healthcare: Develop climate-resilient healthcare infrastructure to ensure uninterrupted services during extreme whether events like floods and droughts.
- Research and development: Invest in research to further elucidate the complex interplay between environmental factors, socioeconomic determinants, and TB transmission dynamics.
By integrating environmental considerations into public health strategies, Nepal can move towards more effective and sustainable TB control.
Take action today! Learn more about tuberculosis prevention and treatment. Contact your local health officials or visit reputable sources for data. Let’s work together to create a healthier future for Nepal.
Analyzing the Correlation Between Environmental Factors and Tuberculosis Prevalence in Nepal
Recent research has illuminated significant correlations between environmental factors—such as land surface temperature,cropland distribution,and urbanization—and the prevalence of tuberculosis (TB) in Nepal. These findings offer insights into how environmental conditions may influence the spread and incidence of this infectious disease.
Land Surface Temperature and Tuberculosis Prevalence
The study examined the relationship between land surface temperature (LST) during both day and night and TB prevalence across Nepal during fiscal years 2020-2023. The analysis revealed statistically significant correlations,indicating that temperature variations may play a role in TB transmission.
Land Surface Temperature Day
Bivariate Local Indicators of Spatial Association (LISA) analysis revealed a notable relationship between daytime land surface temperature (LSTD) and TB prevalence. Specifically, researchers used Moran’s I to measure spatial autocorrelation, identifying clusters of high and low values.
For instance, in FY 2020-2021, specific regions exhibited clustering. Further research could explore how high daytime temperatures might affect human behavior,such as increased indoor crowding during the hottest hours,which could facilitate TB transmission.It’s also possible the increased temperatures affect the viability of the bacteria in the surroundings or the host’s immune response.
Land Surface Temperature Night
The study also found a statistically significant positive correlation between nighttime land surface temperature (LSTN) and TB prevalence across the three fiscal years. The moran’s *I* value steadily climbed, signaling an increasing spatial correlation. What is particularly notable is the consistency of hotspot and cold spot locations, as the analysis showed.
In FY 2020–2021, the Moran’s I was 0.383. High-High clusters were identified in Banke, Rupandehi, Parasi, Parsa, Bara, Rautahat, Makawanpur, Lalitpur, Kabhrepalanchok, and Mahottari, while Low-low clusters appeared in Mustang, Kaski, Solukhumbu, Sankhuwasabha, Taplejung and Panchthar. In FY 2021–2022, Moran’s I increased to 0.420 with hotspots persisting in Banke, kapilbastu, Parsa, Bara, Rautahat, Makawanpur, Lalitpur, Kabhrepalanchok, and Mahottari, while cold spots remained in Solukhumbu, Sankhuwasabha, Taplejung and Panchthar. For FY 2022–2023, Moran’s I rose to 0.425. Hotspots expanded to include Sarlahi, Bhaktapur, and Nuwakot, while cold-spot clusters persisted in Mustang, Kaski, Solukhumbu, Sankhuwasabha, taplejung, and Panchthar.
The persistence of hotspots suggests underlying environmental or socioeconomic factors in those regions that could be contributing to both higher nighttime temperatures and increased TB prevalence. This observation prompts deeper investigation into potential causal relationships, such as how warmer nights may affect sleep patterns, immune function, or other health-related behaviors.
Cropland Distribution and Tuberculosis Prevalence
Beyond temperature, the spatial distribution of cropland also showed a significant correlation with TB prevalence. The presence of High-High clusters signifies areas where abundant cropland coincides with higher TB rates, and this correlation demands that more research be done on the area.
in FY 2020–2021, moran’s I was 0.325 with High-High clusters in Banke, Rupandehi, Parasi, Parsa, Bara, Rautahat, and Mahottari, while Low-Low clusters appeared in mustang, Kaski, Solukhumbu, Sankhuwasabha, Taplejung, Okhaldhunga, bhojpur, terhathum, and Panchthar. in FY 2021–2022, Moran’s I increased to 0.339 with hotspots persisting in Banke, Kapilbastu, parsa, Bara, Rautahat and Mahottari while cold spots remained in Solukhumbu, Sankhuwasabha, Taplejung, Okhaldhunga, Bhojpur, Terhathum, Dhankuta, and Panchthar. For FY 2022–2023, Moran’s I rose to 0.373 with hotspots expanding to include Sarlahi and Bhaktapur. Cold-spot clusters persisted in Mustang, Kaski, Solukhumbu, sankhuwasabha, Taplejung, okhaldhunga, Bhojpur, Terhathum, and Panchthar.
It is indeed significant to note that regions with more cropland may also deal with a lot of other factors that cause TB, as an example, the lack of good nutrition, living in crowded spaces and exposure agricultural chemicals that weaken the immune system.
Urbanization and Tuberculosis Prevalence
Urbanization is also a key factor linked to TB prevalence but the article ends abruptly.
Mapping Tuberculosis: Urbanization, Precipitation, and Spatial Analysis in Nepal
Tuberculosis (TB) remains a significant public health challenge in Nepal. Recent studies are employing spatial analysis to understand the factors influencing TB prevalence, providing crucial insights for targeted interventions. This article delves into emerging patterns and statistical models to dissect the intricate associations between urbanization, precipitation, and TB incidence across the country.
Urbanization and TB Prevalence: A Growing Concern
Urbanization has been identified as a potential driver of TB transmission. Geographic analysis using Moran’s I, a measure of spatial autocorrelation, reveals how clusters of high TB prevalence correlate with urban centers.
- FY 2020–2021: Higher TB cases concentrated in Parsa, Bara, Rautahat, and Mahottari, while lower rates persisted in Solukhumbu, Sankhuwasabha, taplejung, Okhaldhunga, Bhojpur, Terhathum, Dhankuta, and Panchthar.
- FY 2021–2022: “Moran’s I increased to 0.245 with hotspots in Parsa, Bara, rautahat, and Mahottari,” signaling intensifying correlation, while cold spots remained stable.
- FY 2022–2023: “Moran’s I rose to 0.246 with hotspots expanding to include Parasi, Sarlahi, Lalitpur and Bhaktapur,” indicating a geographic spread, with cold spots enduring in mountainous regions like Mustang and Solukhumbu.
This clustering suggests that urban environments, characterized by higher population density and potentially compromised living conditions, may facilitate TB transmission. Further research into the specific dynamics within these hotspots is critical to crafting effective control measures.
The Role of Precipitation: Unpacking Environmental Influences
Along with urbanization, precipitation patterns demonstrate a statistically significant correlation with TB prevalence. The analysis highlights areas where high precipitation coincides with high TB rates.
- FY 2020–2021: Moran’s I was 0.222, showing high-high clusters in Rupandehi, Parasi, Parsa, Bara, Rautahat, Makawanpur, and Mahottari, and low-low clusters in Mustang, Solukhumbu, Sankhuwasabha, Taplejung, Okhaldhunga, Bhojpur, and Terhathum.
- FY 2021–2022: “Moran’s I increased to 0.349 with hotspots identified in Parsa, Bara, Rautahat, Lalitpur, Banke, Kapilbastu, Makawanpur, and Mahottari,” solidifying the link.
- FY 2022–2023: Despite a decrease to 0.104, “the positive spatial autocorrelation persisted. Hotspot clusters expanded to include Parasi,Parsa,Bara,Rautahat,Sarlahi,Makawanpur,Kabhrepalanchok,Nuwakot,Kapilbastu,Lalitpur,and Bhaktapur,” while cold spots remained in Mustang,Solukhumbu,Okhaldhunga,and Bhojpur.
The precise mechanisms through which precipitation influences TB prevalence warrant deeper investigation. Hypotheses include impacts on sanitation, hygiene, and indoor living conditions leading to increased vulnerability among certain populations. Understanding these pathways is crucial in devising targeted interventions.
Statistical Modeling: Quantifying Influences
To quantify the impact of various factors, statistical regression models were employed, including Ordinary Least Squares (OLS), Spatial Error Model (SEM), and Spatial Lag Model (SLM). For fiscal year 2021-2022, the models underscore the significant influence of Land Surface Temperature at Night (LSTN) and urbanization on TB prevalence.
- FY 2021–2022: OLS regression showed LSTN and urbanization accounted for 42.6% of TB prevalence variation (R2 = 0.426). The SLM model “explained 72.1% (R2 = 0.721),” and was favored over SEM due to AIC values (731.009 vs 732.964). Key finding: “LSTN (Coefficient: 1.206) and urbanization (Coefficient: 2.624) continued to show positive autocorrelation with TB prevalence.”
- FY 2022–2023: OLS regression: LSTN, precipitation, and urbanization accounted for 49.9% of the variation (R2 = 0.499). The SLM model explained 69.6% (R2 = 0.696), performing better than the SEM based on AIC values (724.45 vs 726.924).Key finding: “LSTN (Coefficient: 1.750),urbanization (Coefficient: 2.643) and TB prevalence” showed positive autocorrelation.
The Spatial Lag Model (SLM) consistently outperformed other models, suggesting spatial dependencies play a critical role. This highlights the importance of considering neighborhood effects and spatial autocorrelation in TB control strategies. Areas with higher LSTN were also a factor.
Implications and Actionable Insights
The convergence of urbanization, precipitation patterns, and spatial autocorrelation in influencing TB prevalence underscores the need for multifaceted interventions. Public health programs should consider these insights to enhance targeting and effectiveness.
- Targeted Interventions: Prioritize resource allocation to identified “hotspot” regions exhibiting high urbanization levels and specific precipitation patterns.
- Urban Planning and Public Health Integration: Promote healthier living environments through improved sanitation, housing, and access to healthcare services, particularly in rapidly urbanizing areas.
- Climate Resilience: Develop strategies to mitigate potential impacts of changing precipitation patterns on TB transmission, including improved water management and hygiene promotion.
- Further Research: Conduct in-depth studies to elucidate the causal mechanisms linking urbanization, precipitation, and TB, informing evidence-based policy decisions.
By embracing geographic insights and statistical models, we can move towards more effective and equitable TB control efforts in Nepal, safeguarding vulnerable populations and building healthier communities. Contact your local health officials and express your concern and ask what options are available to support TB eradication in your community.
Given the article’s focus on environmental factors contributing to TB prevalence in Nepal, what specific policy recommendations could be implemented to mitigate the impact of climate change on TB transmission?
Tackling Tuberculosis in Nepal: An interview with Dr. Anya Sharma
Tuberculosis (TB) remains a persistent public health challenge in Nepal. Archyde News recently spoke with Dr. Anya Sharma, a leading epidemiologist at the Nepal National Tuberculosis Program, about recent findings linking environmental factors to TB prevalence. Dr. Sharma shares her insights on the hotspots, key drivers, and strategies for combating this disease.
Understanding TB hotspots in Nepal
Archyde: Dr. Sharma, thank you for joining us. Recent studies highlight specific regions in Nepal as TB hotspots. Can you elaborate on these areas and what makes them particularly vulnerable?
Dr. Sharma: Certainly.We’ve consistently seen higher TB prevalence in districts like Banke, Parsa, Rautahat, and Mahottari, particularly in the Terai region. These areas often face challenges such as higher population density, socioeconomic disparities, and limited access to healthcare. Environmental factors, as recent data suggests, might exacerbate the situation.
The Role of Environmental Factors: Temperature, Land Use, and Rainfall
Archyde: The research points to correlations between temperature, land use, and rainfall patterns with TB incidence. how significant are these environmental factors in the overall TB burden?
Dr. Sharma: The correlations are indeed significant. We’ve observed that areas with warmer temperatures, particularly in the densely populated Terai, tend to have higher TB rates. Land use patterns, like the prevalence of cropland and urban areas, also seem to play a role. For instance, urban centers with high population density may facilitate TB transmission. Rainfall patterns can indirectly impact TB by affecting sanitation and perhaps disrupting healthcare access.
Targeted Interventions and community-Based Programs
Archyde: Given these findings, what specific interventions is the National Tuberculosis Programme implementing to address these challenges?
Dr. Sharma: We’re focusing on several key strategies. Firstly, we’re prioritizing resource allocation to high-prevalence districts, ensuring they have adequate diagnostic and treatment facilities.We’re also strengthening community-based TB screening and treatment programs, particularly in densely populated urban areas. Additionally, we are working on climate-resilient healthcare infrastructure to minimize service disruptions during extreme weather events. We are also looking at social determinants such as food security, socio-economic status, and housing.
The Impact of Urbanization on Tuberculosis Transmission
Archyde: Urbanization seems to be a significant factor. How is urbanization altering the landscape of TB transmission in Nepal?
Dr. Sharma: Rapid urbanization often leads to overcrowded living conditions, poor ventilation, and inadequate sanitation, all of which contribute to increased TB transmission. Moreover,urban areas can concentrate vulnerable populations with limited access to healthcare. We’re working on urban-specific TB control strategies that address these unique challenges.
Research and Future Directions in Tuberculosis Control
Archyde: What are the next steps in research and progress to further understand and combat TB in Nepal?
Dr.Sharma: It’s crucial to invest in research to better understand the complex interplay between environmental factors, socioeconomic determinants, and TB transmission dynamics. We need to explore how climate change might impact TB prevalence and develop targeted interventions. Furthermore, research into new diagnostic tools and treatment regimens is essential for achieving our goal of TB elimination.
A Final Thought: Encouraging Community Involvement
Archyde: What message would you like to leave with our readers regarding TB prevention and control in Nepal?
Dr. Sharma: Tuberculosis is a curable disease, but early detection and complete treatment are crucial. I urge everyone to be aware of TB symptoms and seek medical attention if they experience persistent cough, fever, or weight loss. Community participation is vital in TB control. Let’s work together to create a healthier future for Nepal.What are some innovative approaches you think could help raise awareness and improve TB screening rates in your community? Share your thoughts below!